As Skilled Nursing Facilities (SNFs) and Assisted Living Facilities (ALFs) continue to face mounting clinical and regulatory pressures, the need for innovative, resident-centered solutions has never been greater. One area that deserves focused attention is pressure ulcer prevention; an issue that not only impacts resident well-being but also influences a facility’s quality metrics, reimbursement, and reputation.
Mobile wound care services, when combined with predictive analytics and AI-powered imaging, offer a transformative opportunity to reduce pressure ulcer incidence, improve healing outcomes, and ease operational challenges for long-term care teams. For SNF and ALF administrators in the Sacramento area, embracing this model may prove to be a pivotal decision. Head to our services page to learn more about our advanced wound care services for pressure ulcers and other types of wounds.
Understanding the Stakes: Why Pressure Ulcers Demand a Predictive Approach
Pressure ulcers, also known as pressure injuries or bedsores, affect an estimated 2.5 million individuals annually in the U.S. and contribute to more than 60,000 deaths each year. These wounds are not just clinical events; they are markers of systemic care failure that carry significant consequences:
- Survey and regulatory exposure: CMS classifies avoidable pressure ulcers as “never events” and includes them in Five-Star Quality Ratings.
- Reimbursement penalties: Facilities face financial repercussions under the Hospital Readmissions Reduction Program and Medicare Value-Based Purchasing.
- Legal and reputational risk: Pressure ulcers are among the most litigated adverse outcomes in long-term care.
Despite best efforts, traditional care models often miss early tissue damage. By the time a wound becomes visible, tissue necrosis may already be underway. That’s where predictive analytics change the game.
How Predictive Analytics Transforms Pressure Ulcer Prevention
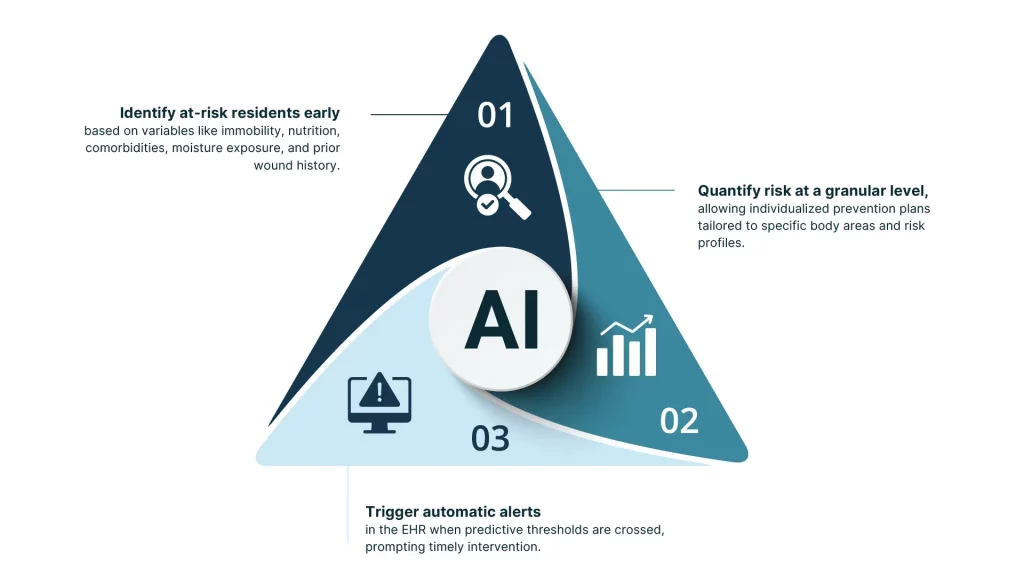
Predictive analytics leverages historical and real-time data to forecast wound risk before clinical symptoms arise. When combined with AI-powered imaging, it allows clinicians to:
- Identify at-risk residents early based on variables like immobility, nutrition, comorbidities, moisture exposure, and prior wound history.
- Quantify risk at a granular level, allowing individualized prevention plans tailored to specific body areas and risk profiles.
- Trigger automatic alerts in the EHR when predictive thresholds are crossed, prompting timely intervention.
This level of precision dramatically reduces the likelihood of pressure injuries forming unnoticed, enabling facilities to intervene before damage becomes irreversible.
Mobile Wound Care: Closing the Loop on Prevention and Treatment
Traditional wound care models often rely on periodic visits by third-party providers, leading to fragmented communication, delayed interventions, and inconsistent documentation. Mobile wound care services offer a better alternative by embedding wound specialists into the facility’s daily clinical operations.
Key advantages include:
- Point-of-care imaging and analysis: AI-guided tools allow clinicians to measure wound depth, stage, and healing trajectory instantly.
- Real-time collaboration: Data is synced with the facility’s EHR and shared across the care team, ensuring everyone is aligned on treatment protocols.
- Treatment without transfer: Residents are assessed and treated in-room, avoiding trauma, discomfort, and costly ambulance rides.
These capabilities not only improve clinical outcomes but also support staff efficiency and interdisciplinary care coordination.
Reducing Readmissions and Improving Clinical Continuity
Pressure ulcers are a leading driver of avoidable hospitalizations from long-term care settings. The progression from Stage I to Stage III or IV often triggers emergency transfers, exposing residents to hospital-acquired infections and disrupting their care continuum.
Mobile wound care services reduce this risk by:
- Providing consistent oversight from wound-certified clinicians who track healing daily or weekly.
- Facilitating rapid escalation through teleconsults with specialists when a wound becomes complex.
- Documenting wound progression in real time, supporting defensible care decisions and better clinical accountability.
This integrated approach translates to fewer hospitalizations, lower treatment costs, and more stable resident experiences.
Enhancing Resident Dignity and Family Confidence
Wound care isn’t just a medical issue. It’s deeply personal. Residents with chronic wounds often suffer from pain, isolation, and loss of dignity. Families, in turn, equate quality wound care with overall facility competency.
By bringing expert care to the bedside, mobile wound teams offer:
- A less invasive experience: No gurneys, no transport vans, no waiting rooms.
- More predictable routines: Treatments are scheduled in coordination with the resident’s care plan, minimizing disruption.
- Greater transparency: Digital imaging and progress reports offer families peace of mind and build trust.
The Bottom Line: Prevention is Profitable
Investing in AI-enhanced mobile wound care isn’t just about clinical outcomes, it’s a high-leverage move for financial performance, staff efficiency, and competitive differentiation. As Sacramento-area SNFs and ALFs prepare for the next phase of care evolution, adopting predictive, tech-enabled wound care should be a cornerstone of their quality and growth strategy.
Learn how our mobile wound care services are helping facilities across Northern California reduce pressure ulcers, improve healing times, and enhance resident satisfaction. Visit our [services page] to explore our advanced wound prevention programs.
Contact us today to schedule your assessment and learn how mobile wound care can transform your clinical outcomes.
